1. Barriers and enablers for the implementation of clinical practice guidelines in China: a mixed-method study
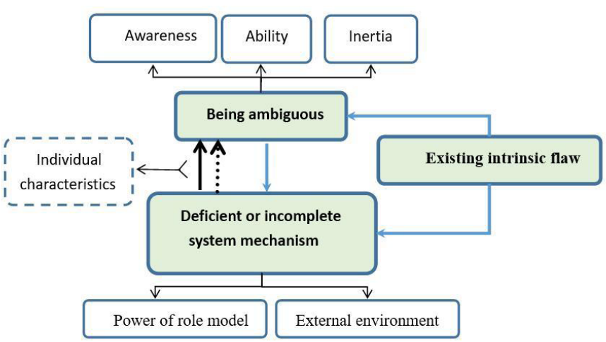
A total of 359 medical practitioners were surveyed and 32 medical practitioners interviewed in 11 cities. Higher frequency and higher ranking of barriers all converged on ‘lack of access’, ‘less convenient’, ‘lack of applicability’ and ‘lack of evidence from Chinese sample’. Higher frequency and higher ranking of enablers converged on ‘Short formats presentation’, ‘Utilisation of various media’, ‘Information visualisation’ and ‘Linking to patient electronic medical records’. There were no relationships between characteristics of respondents with self-reported adherence. This research produced a theoretical understanding of the experience of medical practitioners when using guidelines. Themes identified were as follows: existing intrinsic flaws in guidelines, deficient or incomplete system mechanism and being ambiguous. Our findings provide a comprehensive and culturally sensitive perspective in understanding guideline implementation in China. Strategies addressing those barriers should be further discussed and researched in the future.
https://bmjopen.bmj.com/content/9/9/e026328.full
2 Determinants of successful guideline implementation: a national cross-sectional survey
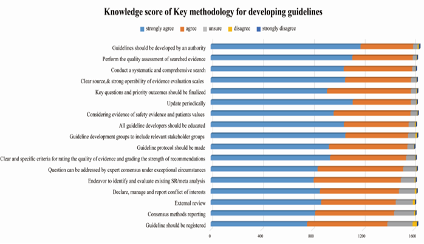
This is a cross‑sectional survey, using multi‑stage stratified typical sampling based on China’s economic regional divisions (the East, the Middle, the West and the Northeast). 2–5 provinces were selected from each region. 2–3 cities were selected in each province, and secondary and tertiary hospitals from each city were included. We developed a questionnaire underpinned by recommended methods for the design and conduct of self‑administered surveys and based on conceptual framework of guideline use, in‑depth related literature analysis, guideline development manuals, related behavior change theory. Finally, multivariate analyses were performed using logistic regression to produce adjusted odds ratios (OR) and 95% confidence intervals (95% CI). There were 1732 participants (87.3% response rate) from 51 hospitals. Of these, 77.2% reported to have used guidelines frequently or very frequently. The key barriers to guideline use were lack of education or training (46.2%), and overly simplistic wording or overly broad scope of recommendations (43.8%). Level of adherence to guidelines was associated with geographical regions (the northeast P < 0.001; the west P = 0.02; the middle P < 0.001 compared with the east), hospital grades (P = 0.028), length of practitioners’ practice (P = 0.006), education background (Ph.D., was associated with geographical regions (the northeast P < 0.001; the west P = 0.02; the middle P < 0.001 compare with the east), hospital grades (P = 0.028), length of practitioners’ practice (P = 0.006), education background (Ph.D., P = 0.027; Master, P = 0.002), evidence‑based medicine skills acquired in work unit (P = 0.012), and medical specialty with the east), hospital grades (P = 0.028), length of practitioners’ practice (P = 0.006), education background (Ph.D., P = 0.027; Master, P = 0.002), evidence‑based medicine skills acquired in work unit (P = 0.012), and medical specialty of practitioner (General Practice, P = 0.006; Surgery, P = 0.043). P = 0.027; Master, P = 0.002), evidence‑based medicine skill practitioner (General Practice, P = 0.006; Surgery, P = 0.043). Despite general acknowledgement of the importance of guidelines, the use of guidelines was not as frequent as might have been expected.